
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
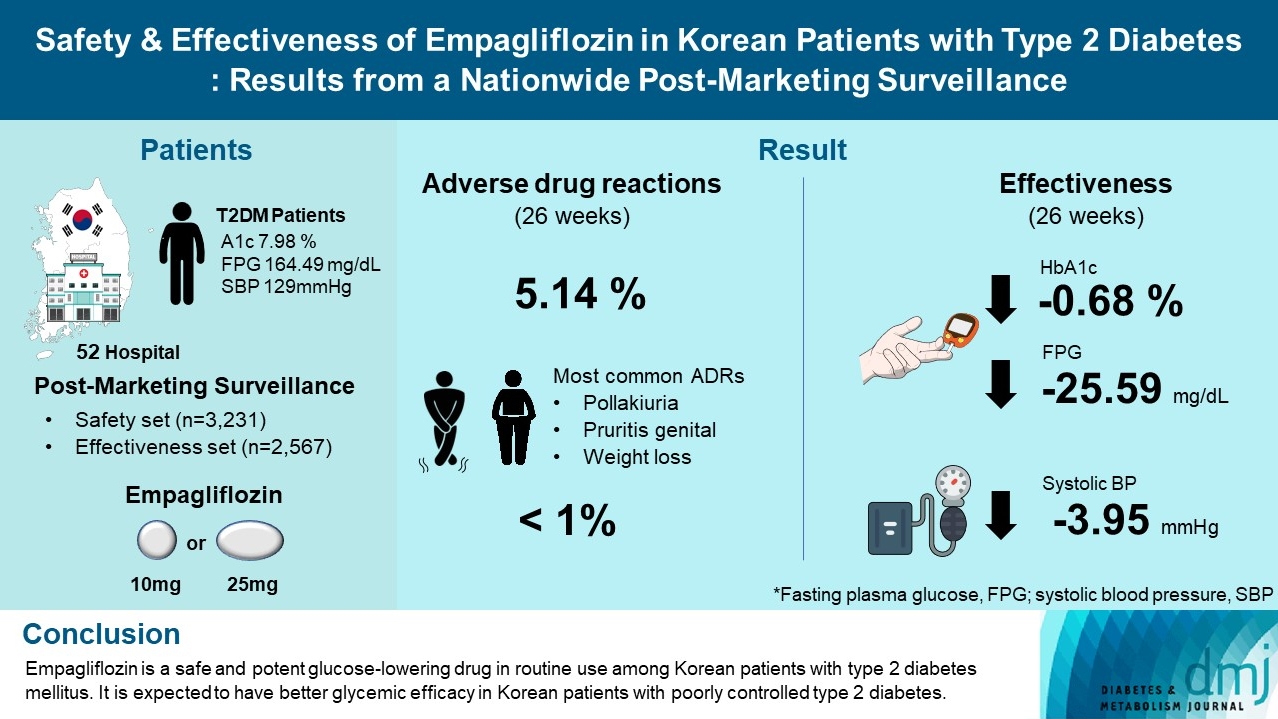
- Safety and Effectiveness of Empagliflozin in Korean Patients with Type 2 Diabetes Mellitus: Results from a Nationwide Post-Marketing Surveillance
- Jun Sung Moon, Nam Hoon Kim, Jin Oh Na, Jae Hyoung Cho, In-Kyung Jeong, Soon Hee Lee, Ji-Oh Mok, Nan Hee Kim, Dong Jin Chung, Jinhong Cho, Dong Woo Lee, Sun Woo Lee, Kyu Chang Won
- Diabetes Metab J. 2023;47(1):82-91. Published online June 20, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0356
- 6,014 View
- 297 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To evaluate the safety and effectiveness of empagliflozin in routine clinical settings, we collected and assessed the clinical profiles of Korean patients with type 2 diabetes mellitus.
Methods
This was a post-marketing surveillance study of empagliflozin 10 and 25 mg. Information on adverse events and adverse drug reactions (ADRs) was collected as safety data sets. Available effectiveness outcomes, including glycosylated hemoglobin (HbA1c) level, fasting plasma glucose, body weight, and blood pressure, were assessed.
Results
The incidence rate of ADRs was 5.14% in the safety dataset (n=3,231). Pollakiuria, pruritis genital, and weight loss were the most common ADRs. ADRs of special interest accounted for only 1.18%, and there were no serious events that led to mortality or hospitalization. In the effectiveness data set (n=2,567), empagliflozin significantly reduced the mean HbA1c level and body weight during the study period by –0.68%±1.39% and –1.91±3.37 kg (both P<0.0001), respectively. In addition, shorter disease duration, absence of dyslipidemia, and higher baseline HbA1c levels were identified as the clinical features characteristic of a “responder” to empagliflozin therapy.
Conclusion
Empagliflozin is a safe and potent glucose-lowering drug in routine use among Korean patients with type 2 diabetes mellitus. It is expected to have better glycemic efficacy in Korean patients with poorly controlled type 2 diabetes mellitus. -
Citations
Citations to this article as recorded by- Evaluation of Efficacy and Safety of Empagliflozin in Bangladeshi Patients with Type 2 Diabetes Mellitus (EFFISAEM Study)
Mohammad Saifuddin, Ajit Kumar Paul, Sultana Marufa Shefin, Md. Jahangir Alam, Shahjada Selim, Sunjida Islam, Tanjina Hossain, Sadiqa Tuqan, Nusrat Sultana, Marufa Mustari, Ramen Chandra Basak, Kazi Ali Aftab, Indrajit Prasad, Mohammad Rafiq Uddin, Shoma
Indian Journal of Endocrinology and Metabolism.2024;[Epub] CrossRef - Comparison of the Pharmacokinetics, Safety, and Tolerability of Two Empagliflozin Formulations in Healthy Korean Subjects
Xu Jiang, Sungyeun Bae, Deok Yong Yoon, Shin Jung Park, Jaeseong Oh, Joo-Youn Cho, Kyung-Sang Yu
Drug Design, Development and Therapy.2023; Volume 17: 2137. CrossRef - Comparative safety of different sodium-glucose transporter 2 inhibitors in patients with type 2 diabetes: a systematic review and network meta-analysis of randomized controlled trials
Chun Xing Li, Li Yan Liu, Chen Xiao Zhang, Xu Hua Geng, Si Meng Gu, Yu Qiao Wang, Hua Liu, Qing Xie, Shuo Liang
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Evaluation of Efficacy and Safety of Empagliflozin in Bangladeshi Patients with Type 2 Diabetes Mellitus (EFFISAEM Study)
- Drug/Regimen
- Efficacy and Safety of Treatment with Quadruple Oral Hypoglycemic Agents in Uncontrolled Type 2 Diabetes Mellitus: A Multi-Center, Retrospective, Observational Study
- Jun Sung Moon, Sunghwan Suh, Sang Soo Kim, Heung Yong Jin, Jeong Mi Kim, Min Hee Jang, Kyung Ae Lee, Ju Hyung Lee, Seung Min Chung, Young Sang Lyu, Jin Hwa Kim, Sang Yong Kim, Jung Eun Jang, Tae Nyun Kim, Sung Woo Kim, Eonju Jeon, Nan Hee Cho, Mi-Kyung Kim, Hye Soon Kim, Il Seong Nam-Goong, Eun Sook Kim, Jin Ook Chung, Dong-Hyeok Cho, Chang Won Lee, Young Il Kim, Dong Jin Chung, Kyu Chang Won, In Joo Kim, Tae Sun Park, Duk Kyu Kim, Hosang Shon
- Diabetes Metab J. 2021;45(5):675-683. Published online August 12, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0107

- 35,402 View
- 367 Download
- 9 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
Background Only few studies have shown the efficacy and safety of glucose-control strategies using the quadruple drug combination. Therefore, the aim of the present study was to investigate the usefulness of the quadruple combination therapy with oral hypoglycemic agents (OHAs) in patients with uncontrolled type 2 diabetes mellitus (T2DM).
Methods From March 2014 to December 2018, data of patients with T2DM, who were treated with quadruple hypoglycemic medications for over 12 months in 11 hospitals in South Korea, were reviewed retrospectively. We compared glycosylated hemoglobin (HbA1c) levels before and 12 months after quadruple treatment with OHAs. The safety, maintenance rate, and therapeutic patterns after failure of the quadruple therapy were also evaluated.
Results In total, 357 patients were enrolled for quadruple OHA therapy, and the baseline HbA1c level was 9.0%±1.3% (74.9±14.1 mmol/mol). After 12 months, 270 patients (75.6%) adhered to the quadruple therapy and HbA1c was significantly reduced from 8.9%±1.2% to 7.8%±1.3% (mean change, −1.1%±1.2%;
P <0.001). The number of patients with HbA1c <7% increased significantly from 5 to 68 (P <0.005). In addition, lipid profiles and liver enzyme levels were also improved whereas no changes in body weight. There was no significant safety issue in patients treated with quadruple OHA therapy.Conclusion This study shows the therapeutic efficacy of the quadruple OHA regimen T2DM and demonstrates that it can be an option for the management of T2DM patients who cannot use insulin or reject injectable therapy.
-
Citations
Citations to this article as recorded by- Estimating Type 2 Diabetes Prevalence: A Model of Drug Consumption Data
Rita Oliveira, Matilde Monteiro-Soares, José Pedro Guerreiro, Rúben Pereira, António Teixeira-Rodrigues
Pharmacy.2024; 12(1): 18. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Effectiveness and safety of teneligliptin added to patients with type 2 diabetes inadequately controlled by oral triple combination therapy: A multicentre, randomized, double‐blind, and placebo‐controlled study
Minyoung Lee, Woo‐je Lee, Jae Hyeon Kim, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(6): 1105. CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - Glycaemic control with add‐on thiazolidinedione or a sodium‐glucose co‐transporter‐2 inhibitor in patients with type 2 diabetes after the failure of an oral triple antidiabetic regimen: A 24‐week, randomized controlled trial
Jaehyun Bae, Ji Hye Huh, Minyoung Lee, Yong‐Ho Lee, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2021; 23(2): 609. CrossRef
- Estimating Type 2 Diabetes Prevalence: A Model of Drug Consumption Data
- Complications
- The Association between Pancreatic Steatosis and Diabetic Retinopathy in Type 2 Diabetes Mellitus Patients
- Jee Sun Jeong, Mee Kyung Kim, Kyung Do Han, Oak Kee Hong, Ki-Hyun Baek, Ki-Ho Song, Dong Jin Chung, Jung-Min Lee, Hyuk-Sang Kwon
- Diabetes Metab J. 2018;42(5):425-432. Published online August 9, 2018
- DOI: https://doi.org/10.4093/dmj.2017.0107
- 4,124 View
- 43 Download
- 5 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Whether pancreatic steatosis has a local or systemic effect, like ectopic fat of other major organs, remains unknown. Data on the influence of pancreatic steatosis on microvascular complication are rare. Therefore, we investigated the relationship between pancreatic steatosis and diabetic retinopathy (DR) in patients with type 2 diabetes mellitus (T2DM).
Methods The attenuation of three pancreatic regions (head, body, and tail) and the spleen (S) in 186 patients with T2DM was measured using non-enhanced computed tomography imaging. We used three parameters for the assessment of pancreatic steatosis (‘P’ mean: mean attenuation of three pancreatic regions; P–S: difference between ‘P’ mean and ‘S’; P/S: the ‘P’ mean to ‘S’ ratio). The presence of DR was assessed by an expert ophthalmologist using dilated fundoscopy.
Results The average P mean was 29.02 Hounsfield units (HU), P–S was −18.20 HU, and P/S was 0.61. The three pancreatic steatosis parameters were significantly associated with the prevalence of DR in non-obese T2DM patients. In the non-obese group, the odds ratios of P mean, P–S, and P/S for the prevalence of DR, after adjustment for age, sex, and glycosylated hemoglobin level, were 2.449 (
P =0.07), 2.639 (P =0.04), and 2.043 (P =0.02), respectively.Conclusion In this study, pancreatic steatosis was significantly associated with DR in non-obese patients with T2DM. Further studies are necessary to clarify the causal relationship between pancreatic steatosis and the development of DR.
-
Citations
Citations to this article as recorded by- Intra‐pancreatic fat is associated with continuous glucose monitoring metrics
Yutong Liu, Wandia Kimita, Xiatiguli Shamaitijiang, Loren Skudder‐Hill, Ivana R. Sequeira‐Bisson, Maxim S. Petrov
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Association between Intrapancreatic Fat Deposition and Lower High-Density Lipoprotein Cholesterol in Individuals with Newly Diagnosed T2DM
Jianliang Wang, Qingyun Cai, Xiaojuan Wu, Jiaxuan Wang, Xiaona Chang, Xiaoyu Ding, Jia Liu, Guang Wang, Muhittin Yurekli
International Journal of Endocrinology.2023; 2023: 1. CrossRef - The comparison of pancreatic and hepatic steatosis in healthy liver donor candidates
Bedriye Koyuncu Sokmen, Tolga Sahin, Alihan Oral, Erdem Kocak, Nagihan Inan
Scientific Reports.2021;[Epub] CrossRef - Computed Tomography-Estimated Pancreatic Steatosis is Associated with Carotid Plaque in Type 2 Diabetes Mellitus Patients: A Cross-Sectional Study from China
Pengtao Sun, Chunzhi Fan, Rengui Wang, Tongwei Chu, Xiaoli Sun, Dongxue Zhang, Xuechao Du
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 1329. CrossRef
- Intra‐pancreatic fat is associated with continuous glucose monitoring metrics
- Others
- Comparison of Vildagliptin and Pioglitazone in Korean Patients with Type 2 Diabetes Inadequately Controlled with Metformin
- Jong Ho Kim, Sang Soo Kim, Hong Sun Baek, In Kyu Lee, Dong Jin Chung, Ho Sang Sohn, Hak Yeon Bae, Mi Kyung Kim, Jeong Hyun Park, Young Sik Choi, Young Il Kim, Jong Ryeal Hahm, Chang Won Lee, Sung Rae Jo, Mi Kyung Park, Kwang Jae Lee, In Joo Kim
- Diabetes Metab J. 2016;40(3):230-239. Published online April 5, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.3.230
- 5,221 View
- 48 Download
- 13 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background We compared the efficacies of vildagliptin (50 mg twice daily) relative to pioglitazone (15 mg once daily) as an add-on treatment to metformin for reducing glycosylated hemoglobin (HbA1c) levels in Korean patients with type 2 diabetes.
Methods The present study was a multicenter, randomized, active-controlled investigation comparing the effects of vildagliptin and pioglitazone in Korean patients receiving a stable dose of metformin but exhibiting inadequate glycemic control. Each patient underwent a 16-week treatment period with either vildagliptin or pioglitazone as an add-on treatment to metformin.
Results The mean changes in HbA1c levels from baseline were –0.94% in the vildagliptin group and –0.6% in the pioglitazone group and the difference between the treatments was below the non-inferiority margin of 0.3%. The mean changes in postprandial plasma glucose (PPG) levels were –60.2 mg/dL in the vildagliptin group and –38.2 mg/dL in the pioglitazone group and these values significantly differed (
P =0.040). There were significant decreases in the levels of total, low density lipoprotein, high density lipoprotein (HDL), and non-HDL cholesterol in the vildagliptin group but increases in the pioglitazone group. The mean change in body weight was –0.07 kg in the vildagliptin group and 0.69 kg in the pioglitazone group, which were also significantly different (P =0.002).Conclusion As an add-on to metformin, the efficacy of vildagliptin for the improvement of glycemic control is not inferior to that of pioglitazone in Korean patients with type 2 diabetes. In addition, add-on treatment with vildagliptin had beneficial effects on PPG levels, lipid profiles, and body weight compared to pioglitazone.
-
Citations
Citations to this article as recorded by- Factors contributing to the adverse drug reactions associated with the dipeptidyl peptidase-4 (DPP-4) inhibitors: A scoping review
Swetha R. Reghunath, Muhammed Rashid, Viji Pulikkel Chandran, Girish Thunga, K.N. Shivashankar, Leelavathi D. Acharya
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(7): 102790. CrossRef - Efficacy and safety of evogliptin in patients with type 2 diabetes and non‐alcoholic fatty liver disease: A multicentre, double‐blind, randomized, comparative trial
Eugene Han, Ji Hye Huh, Eun Y. Lee, Ji C. Bae, Sung W. Chun, Sung H. Yu, Soo H. Kwak, Kyong S. Park, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(4): 752. CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - The rs12617336 and rs17574 Dipeptidyl Peptidase-4 Polymorphisms Are Associated With Hypoalphalipoproteinemia and Dipeptidyl Peptidase-4 Serum Levels: A Case-Control Study of the Genetics of Atherosclerotic Disease (GEA) Cohort
Gilberto Vargas-Alarcón, María del Carmen González-Salazar, Christian Vázquez-Vázquez, Adrián Hernández-Díaz Couder, Fausto Sánchez-Muñoz, Juan Reyes-Barrera, Sergio A. Criales-Vera, Marco Sánchez-Guerra, Citlalli Osorio-Yáñez, Rosalinda Posadas-Sánchez
Frontiers in Genetics.2021;[Epub] CrossRef - Reduction in HbA1c with SGLT2 inhibitors vs. DPP-4 inhibitors as add-ons to metformin monotherapy according to baseline HbA1c: A systematic review of randomized controlled trials
A.J. Scheen
Diabetes & Metabolism.2020; 46(3): 186. CrossRef - Combination Therapy of Oral Hypoglycemic Agents in Patients with Type 2 Diabetes Mellitus
Min Kyong Moon
The Journal of Korean Diabetes.2018; 19(1): 23. CrossRef - Comparative Cardiovascular Risks of Dipeptidyl Peptidase-4 Inhibitors: Analyses of Real-world Data in Korea
Kyoung Hwa Ha, Bongseong Kim, Hae Sol Shin, Jinhee Lee, Hansol Choi, Hyeon Chang Kim, Dae Jung Kim
Korean Circulation Journal.2018; 48(5): 395. CrossRef - Safety and efficacy of low dose pioglitazone compared with standard dose pioglitazone in type 2 diabetes with chronic kidney disease: A randomized controlled trial
Bancha Satirapoj, Khanin Watanakijthavonkul, Ouppatham Supasyndh, Stephen L Atkin
PLOS ONE.2018; 13(10): e0206722. CrossRef - Combination therapy of oral hypoglycemic agents in patients with type 2 diabetes mellitus
Min Kyong Moon, Kyu Yeon Hur, Seung-Hyun Ko, Seok-O Park, Byung-Wan Lee, Jin Hwa Kim, Sang Youl Rhee, Hyun Jin Kim, Kyung Mook Choi, Nan-Hee Kim
The Korean Journal of Internal Medicine.2017; 32(6): 974. CrossRef - Combination Therapy of Oral Hypoglycemic Agents in Patients with Type 2 Diabetes Mellitus
Min Kyong Moon, Kyu-Yeon Hur, Seung-Hyun Ko, Seok-O Park, Byung-Wan Lee, Jin Hwa Kim, Sang Youl Rhee, Hyun Jin Kim, Kyung Mook Choi, Nan-Hee Kim
Diabetes & Metabolism Journal.2017; 41(5): 357. CrossRef - Efficacy and safety of adding evogliptin versus sitagliptin for metformin‐treated patients with type 2 diabetes: A 24‐week randomized, controlled trial with open label extension
Sang‐Mo Hong, Cheol‐Young Park, Dong‐Min Hwang, Kyung Ah Han, Chang Beom Lee, Choon Hee Chung, Kun‐Ho Yoon, Ji‐Oh Mok, Kyong Soo Park, Sung‐Woo Park
Diabetes, Obesity and Metabolism.2017; 19(5): 654. CrossRef - Antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus 2017: a position statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 947. CrossRef - Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 337. CrossRef
- Factors contributing to the adverse drug reactions associated with the dipeptidyl peptidase-4 (DPP-4) inhibitors: A scoping review
- Response: Association between Diabetic Polyneuropathy and Chronic Complications in Type 2 Diabetic Patients (Diabetes Metab J 2011;35:390-6)
- Jin Ook Chung, Dong Hyeok Cho, Dong Jin Chung, Min Young Chung
- Diabetes Metab J. 2011;35(6):640-641. Published online December 26, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.6.640
- 2,567 View
- 26 Download
- Association between Diabetic Polyneuropathy and Cardiovascular Complications in Type 2 Diabetic Patients
- Jin Ook Chung, Dong Hyeok Cho, Dong Jin Chung, Min Young Chung
- Diabetes Metab J. 2011;35(4):390-396. Published online August 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.4.390
- 3,424 View
- 36 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Diabetes mellitus is a major independent risk factor for cardiovascular disease (CVD), but high cardiovascular risk in diabetes mellitus patients is not completely explained by clustering traditional risk factors. Recently, associations between diabetic polyneuropathy (DPN) and macrovasculopathy have been suggested. We aimed to assess associations between DPN and cardiovascular complications in type 2 diabetic patients.
Methods Microvascular and cardiovascular complications were evaluated in 1,041 type 2 diabetic patients.
Results In patients with DPN, the age, prevalence of hypertension, diabetes duration, systolic blood pressure, pulse pressure, and hemoglobin glycation (HbA1c) levels were significantly higher, while the high density lipoprotein cholesterol (HDL-C) levels were lower than in those without DPN. The prevalence of CVD was higher in patients with DPN. In multivariate analysis, DPN was independently associated with CVD (odds ratio, 1.801; 95% confidence interval, 1.009 to 3.214).
Conclusion Our results showed that DPN was associated with a high prevalence of cardiovascular disease in type 2 diabetic patients, but further studies are needed to investigate the causative nature of associations between DPN and CVD.
-
Citations
Citations to this article as recorded by- The Presence of Clonal Hematopoiesis Is Negatively Associated with Diabetic Peripheral Neuropathy in Type 2 Diabetes
Tae Jung Oh, Han Song, Youngil Koh, Sung Hee Choi
Endocrinology and Metabolism.2022; 37(2): 243. CrossRef - Diabetic Peripheral Neuropathy Is Associated With Higher Systolic Blood Pressure in Adults With Type 2 Diabetes With and Without Hypertension in the Chinese Han Population
Lingning Huang, Yongze Zhang, Yunmin Wang, Ximei Shen, Sunjie Yan
Canadian Journal of Diabetes.2020; 44(7): 615. CrossRef - Characterizing distal peripheral neuropathy in type 2 diabetes mellitus in a semi-urban community setting in Peru
Meera F Iyengar, Antonio Bernabe-Ortiz
Journal of Global Health Reports.2019;[Epub] CrossRef - Cardiovascular disease predicts diabetic peripheral polyneuropathy in subjects with type 2 diabetes: A 10-year prospective study
Juan Ybarra-Muñoz, Jeronimo Jurado-Campos, Maria Garcia-Gil, Edurne Zabaleta-del-Olmo, Teresa Mir-Coll, Adelaida Zabalegui, Josep Vidal, June H Romeo
European Journal of Cardiovascular Nursing.2016; 15(4): 248. CrossRef - Diabetic polyneuropathy and the risk of developing diabetic retinopathy: a nationwide, population‐based study
I‐Chan Lin, Yuan–Hung Wang, Cheng‐Li Lin, Yen‐Jung Chang, Shwu‐Huey Lee, I‐Jong Wang
Acta Ophthalmologica.2015; 93(8): 713. CrossRef - Diabetic Peripheral Neuropathy in Ambulatory Patients with Type 2 Diabetes in a General Hospital in a Middle Income Country: A Cross-Sectional Study
María de los Angeles Lazo, Antonio Bernabé-Ortiz, Miguel E. Pinto, Ray Ticse, German Malaga, Katherine Sacksteder, J. Jaime Miranda, Robert H. Gilman, Leighton R. James
PLoS ONE.2014; 9(5): e95403. CrossRef - The co-occurrence of myocardial dysfunction and peripheral insensate neuropathy in a streptozotocin-induced rat model of diabetes
Maria N Marangoni, Scott T Brady, Shamim A Chowdhury, Mariann R Piano
Cardiovascular Diabetology.2014;[Epub] CrossRef - Neovascularization in diabetes and its complications. Unraveling the angiogenic paradox
Paulo Zoé Costa, Raquel Soares
Life Sciences.2013; 92(22): 1037. CrossRef - Diabetic Peripheral Neuropathy in Type 2 Diabetes Mellitus in Korea
Seung-Hyun Ko, Bong-Yun Cha
Diabetes & Metabolism Journal.2012; 36(1): 6. CrossRef - Epidemiology of Micro- and Macrovascular Complications of Type 2 Diabetes in Korea
Jung Hee Kim, Dae Jung Kim, Hak Chul Jang, Sung Hee Choi
Diabetes & Metabolism Journal.2011; 35(6): 571. CrossRef
- The Presence of Clonal Hematopoiesis Is Negatively Associated with Diabetic Peripheral Neuropathy in Type 2 Diabetes
- Chronic Complications in Adult Diabetic Patients with and without GAD Antibody.
- Jin Ook Chung, Dong Hyeok Cho, Dong Jin Chung, Min Young Chung
- Korean Diabetes J. 2009;33(2):124-133. Published online April 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.2.124
- 2,081 View
- 18 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Although the majority of diabetes mellitus (DM) patients diagnosed as adults have non-autoimmune forms of the disease, islet autoimmunity is encountered in some patients initially thought to have type 2 DM. The phenotype of DM patients with glutamic acid decarboxylase (GAD) antibodies is different from that of patients with GAD antibody-negative type 2 DM, with features such as relative leanness and hyperglycemia which may influence the development of complications. We sought to compare the prevalence of chronic complications in patients with and without the GAD antibody. METHODS: We recruited 427 patients (M: 218, F: 209) that were clinically diagnosed with type 2 DM after the age of 35 years. We measured GAD antibody and assessed the factors associated with chronic microvascular and macrovascular complications. RESULTS: Of these patients, 26 were GAD antibody-positive. The patients with GAD antibody had lower systolic blood pressure, higher high-density lipoprotein cholesterol value, and lower level of fasting and stimulated C-peptide than patients without GAD antibody (P < 0.05). Also, the patients with GAD antibody had lower prevalence of retinopathy compared with the patients without GAD antibody (19.2 vs. 47.9%; P < 0.05). The prevalence of nephropathy, peripheral neuropathy and cardiovascular autonomic neuropathy did not differ between the groups. In addition, the prevalence of coronary heart disease, cerebrovascular disease and peripheral arterial disease did not differ between the two groups. CONCLUSION: This study suggests that diabetic patients with GAD antibody have a lower risk for the development of retinopathy compared with patients without GAD antibody. -
Citations
Citations to this article as recorded by- Relationship between β-Cell Autoantibodies and Their Combination with Anthropometric and Metabolic Components and Microvascular Complications in Latent Autoimmune Diabetes in Adults
Tomislav Bulum, Marijana Vučić Lovrenčić, Jadranka Knežević Ćuća, Martina Tomić, Sandra Vučković-Rebrina, Lea Duvnjak
Biomedicines.2023; 11(9): 2561. CrossRef
- Relationship between β-Cell Autoantibodies and Their Combination with Anthropometric and Metabolic Components and Microvascular Complications in Latent Autoimmune Diabetes in Adults
- A Case of Recurrent Hypoglycemic Hemiparesis in an Adult with Type 1 Diabetes Mellitus.
- Kyoung Min Kim, Se Hun Kang, Se In Hong, Dong Hyeok Cho, Ho Cheol Kang, Dong Jin Chung, Min Young Chung
- Korean Diabetes J. 2006;30(2):136-139. Published online March 1, 2006
- DOI: https://doi.org/10.4093/jkda.2006.30.2.136
- 1,846 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Transient hypoglycemic hemiparesis is a rare but important presentation of hypoglycemia that is frequently misdiagnosed as stroke. The development of hemiparesis as a result of hypoglycemia was first described in 1928. Thereafter over the years, several cases have been sporadically reported in Korea, but case reports of recurrent hypoglycemic hemiparesis are rare. We recently experienced a case of recurrent hypoglycemic hemiparesis in an adult with type 1 diabetes mellitus. A 30-year-old woman with type 1 diabetes receiving daily multiple subcutaneous insulin injections was admitted with right hemiparesis. She had had admitted with the same symptom and recovered with oral carbohydrates in twice 2 years ago. Her clinical course improved over 2 hours after infusion of dextrose solution. Further investigations such as CT, MRI and MRA revealed no abnormality
- Platelet Aggregability in Type 2 Diabetics.
- Chang Hun Lee, Nam Il Cheon, Yeon Sang Lee, Dong Hyeok Cho, Hyun Ho Shin, Jung Min Kim, Dae Ho Lee, Dong Jin Chung, Min Young Chung, Tai Hee Lee
- Korean Diabetes J. 2000;24(3):300-309. Published online January 1, 2001
- 1,075 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Increased platelet aggregability is known to be one of the important risk factors for diabetic vascular complications. The relationship between platelet aggregability and diabetic macrovascular complications, varying severity of diabetic microvascular complications and other possible factors was evaluated in Korean adults. METHODS: Platelet aggregability was measured with platelet rich plasma by addition of adenosine diphosphate (ADP) in 45 cases. Normal control group (n=15) was compared with diabetics without macrovascular complications (n=15), diabetics with macrovascular complications (n=15) and several groups divided accoring to the severity of microvascular complications. RESULTS: 1) The mean maximum value of platelet aggregation was 70.3+/-5.3% in control group, and 80.0+/-7.3% in diabetics (p<0.005). 2) The mean maximum value of platelet aggregation was 78.0+/-5.5% in diabetics without macrovascular complications and 83.5+/-7.1% in diabetics with macrovascular complications (p=0.093). 3) The mean maximum value of platelet aggregation was 77.0+/-5.1% in normoproteinuria group, 78.1+/-7.3% in microproteinuria group, and 82.9+/-6.2% in overt proteinuria group (p=0.083). 4) The mean maximum value of platelet aggregation was 77.2+/-6.8% in diabetes without neuropathy group and 82.9+/-6.2% in diabetes with neuropathy group (p=0.114). 5) The mean maximum value of platelet aggregation was 79.3+/-4.9% in diabetes with normal funduscopic findings, 80.2+/-7.3% in diabetes with background retinopathy and 81.6+/-7.9% in diabetes with proliferative retinopathy (p=0.852). 6) Blood glucose showed positive correlations with the mean maximum platelet aggregation ( =0.529, p<0.005). CONCLUSION: The elevated mean maximum value of platelet aggregation was found in diabetics and there were no significant differences between macrovascular complications and between varying severity of retinopathy, neuropathy and proteinuria. Blood glucose showed positive correlations with mean maximum platelet aggregation. Hyperglycemia was a major risk factor affecting platelet aggregation in diabetics and its control may play an important role in prevention of diabetic vascular complications.
- Lipoprotein (a) Level and Vascular Complications in NIDDM.
- Ji Youn Kim, Mung Su Kim, Joung Min Kim, Jai Hong Park, Joung Hun Lee, Seung Won Yang, Dong Jin Chung, Min Young Chung, Tai Hee Lee
- Korean Diabetes J. 1998;22(1):65-73. Published online January 1, 2001
- 976 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The risk of atherosclerosis is increased in subjects with diabetes mellitus. Lipoprotein(a) [Lp(a)] is an independent risk factor for atherosclerotic vascular disease in subjects without diabetes. The contribution of Lp(a) to the increased risk for atherosclerosis and diabetic complications in subjects with diabetes is not well known. In this report we examined the relationship between Lp(a) levels and development of vascular (macro- and microvascular) complications, and the relationship between Lp(a) and other risk factors for vascular complications in subjects with non-insulin-dependent diabetes mellitus(NIDDM), METHODS: For this study we evaluated 152 patients with NIDDM(72 women and 80 men). Lp(a) level was measured with N-Latex Lp(a) Reagent. Electrocardiography, coronary angiography, brain CT/MRI, doppler velocimetry and peripheral angiography were done for diagnosis of macravascular complieations, and fundus camera, nerve conduction velocity, BBV (beat to beat variation), VPT(vibration perception threshold) and 24-hour urine protein amount were examined for diagnosis of microvascular complications. RESULTS: Lp(a) levels in subjects with ischemic heart disease, cerebrovascular disease and diabetic retinopathy were significantly higher than those in subjects without above mentioned diseases. ApoB/ApoA1 ratio and LDL-cholesterol levels in subjects with Lp(a) level>30mg/dL were significantly higher than those in subjects with Lp(a) level 30mg/dL, and Lp(a) has a positive correlation with ApoB/ApoA1 ratio and LDL-cholesterol in NIDDM patients with vasculopathy. CONCLUSION: These results suggest that high Lp(a) levels seem to be associated with macrovascular and microvascular(especially with retinopathy) complications in subjects with NIDDM and Lp(a) level should be measured in the NIDDM with high level of ApoB/ApoA1 ratio and/or LDL-eholesterol.

 KDA
KDA
 First
First Prev
Prev





